Depression: A Role for Dietary Supplements in It’s Treatment
By Gene Bruno, MS, MHS
Are you depressed? If so, you’re not the only one. In fact, approximately 20.9...
Depression: Functional Medicine Approach
By Ronald Grisanti, DC, DABCO, DACBN, MS
 Depression is considered the most dreaded condition of mankind. What makes depression so awful is the sad fact that it is the one disease devoid of hope in the minds of many who suffer with this global epidemic.
Depression is considered the most dreaded condition of mankind. What makes depression so awful is the sad fact that it is the one disease devoid of hope in the minds of many who suffer with this global epidemic.
Unlike debilitating diseases like arthritis, which shows it's ugly face by causing pain, depression is a silent enemy afflicting millions every year.
My goal in this article is to prepare and educate you on a few of the common triggers of depression.
These are not original thoughts on the subject of depression but are in fact documented peer-reviewed research proving the existence of a world of information kept under "lock and key" contributing to a sea of suffering and mental anguish.
You will soon discover information that will change your life and the life of your family, friends, and patients.
Depression is a national and global epidemic. Just in the United States alone there are over 12 million people who suffer with depression, and that number is rising at an alarming rate. The costs to the American public are enormous.
The following are just a few of the common causes of depression. If you want to get better and bring happiness and joy back into your life, then you owe it to yourself to be absolutely certain that you have each of the following causes thoroughly checked.
Here is the first area you need to have checked:
Approximately 10%-15% of patients with depression have a thyroid hormone deficiency. Now I must emphasize to you that the testing of your thyroid MUST include the following:
Thyroid-stimulating hormone (TSH)
Free serum thyroxine (fT4)
Free triiodothyroine (fT3)
Reverse T3 (rT3)
Anti-thyroglobulin antibodies (anti-TG)
Anti-thyroid peroxidase antibodies (anti-TPO)
Anything less than this is simply unacceptable.
It is well documented that the evaluation of only TSH is inadequate as a means of testing your thyroid. If you have been told by your physician that your thyroid is fine and have not had the above tests ordered, then think again...your physician DOES NOT have all the facts.
Obtaining a comprehensive thyroid panel is essential to rule out thyroid disorder as a possible cause of depression. The medical literature has discovered a link between low T3 and long standing depression. In fact the common treatment of hypothyroidism with Synthroid (a T4-only thyroid medication) may be contributing to an increase in depressive symptoms due to its inability to address a deficient T3.
A comprehensive thyroid panel will also test the possibility of you suffering from a thyroid autoimmune/depression syndrome. The medical literature has found women with high levels
of anti-thyroid peroxidase (anti-TPO) antibodies to be more vulnerable to depression. A recent German study concluded: "in cases of repeated depressive episodes, it seems necessary not only to get lab testing for TSH, T3, and T4 but also to assess the autoimmune status of the thyroid gland (autoantibodies)."
As you have read, it is CRITICAL that you ask your physician to do a comprehensive thyroid panel. DO NOT settle for a TSH test alone. The cause of your depression just may be found with a thyroid problem.
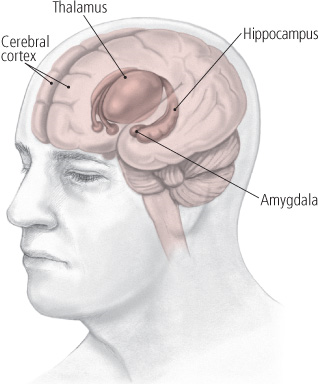
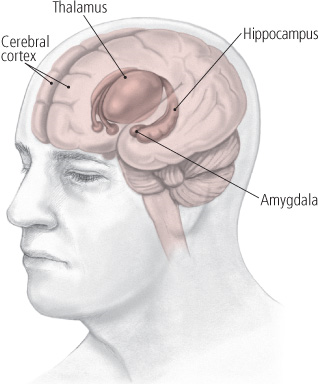
Depression has been linked to disruptions in the body's stress center the hypothalamic pituitary adrenal (HPA) axis. The HPA is a complex communication system between the hypothalmus, the pituitary gland, and the adrenal glands.
The hypothalamus is a region of the brain that controls an immense number of bodily functions including, but not limited to, emotions, behavior, pain, and pleasure.
The pituitary gland is again divided into two distinct portions: the anterior (front) pituitary and the posterior (back) pituitary portions. For the sake of this article, I will only discuss the significance of the anterior pituitary and its relation to depression.
The anterior pituitary produces six very important hormones. Each has a different and distinct function necessary for maintaining health and well-being. One hormone of special interest for the topic of depression is called Adrenocorticotropin. Adrenocorticotropin is responsible for causing the adrenal glands to produce the well-known stress hormones called cortisol and DHEA.
Now with some basic physiology under your belt, here is what happens to a person suffering with depression.
First, when a person experiences some powerful depressing thought, the hypothalamus is sent a signal to wake the pituitary up telling it to produce some of its hormones. The hypothalmus is basically a collecting center for information concerned with the well-being of the body, and in turn much of this information is used to stimulate the pituitary to produce its hormones.
The one hormone just discussed is called Adrenocorticotropin. This in turn sends a signal to the adrenal glands to produce more and more of its hormones. Adrenal gland secretion of the hormones cortisol and DHEA has been directly tied to stress and other emotional factors.
A strong relationship between the overproduction of cortisol and mood variations has been established in both depressed and healthy individuals. As with many of the body's physiological responses, balance is the key. Overactivity of the body's stress system is associated with anxiety, insomnia, loss of libido, while underactivity is linked to depression with accompanying fatigue, lethargy, and indifference.
Depressed individuals often exhibit trouble in the normal relationship between the hypothalmic, pituitary, and adrenal glands. A hyperactive Hypothalamic-Pituitary-Adrenal axis may likely result in a hypersecretion (too much) of cortisol, which in turn will also result in depressive symptoms.
It is important to know how your hypothalmic pituitary adrenal (HPA) axis is functioning. With that information in hand, your physician will be in a better position to outline a patient specific treatment.
Here are two excellent labs that I presently use:
DiagnosTechs and Genova
As the incidence of depression reaches epidemic proportions, I sometimes wonder how one can overlook or may I say ignore the research documenting known causes that can be easily identified and treated.
Another common cause is the relationship between nutrient deficiencies, chemical toxins, and depression.
The medical literature is "over-flowing" with peer-reviewed abstracts proving beyond a shadow of a doubt that depression, nutritional deficiencies, and chemical toxicities are linked.
Our bodies require optimal amounts of trace minerals such as magnesium, zinc, and vanadium (to name a few) to function. Not too much and not too little... just the right balance. Excesses or deficiencies of specific minerals can set off symptoms of depression. For instance, low levels of zinc are associated with resistant depression. Deficiencies of magnesium can bring on a wide range of psychiatric symptoms related to depression and psychosis. Research has revealed a link between high levels of the mineral vanadium and manic symptoms.

One of the big problems with chemicals is they have this nasty ability to sneak up on you and when you least expect it. Most of the chemical sensitivities sneak up on a person over a period of weeks, months or years slowly damaging your detoxification pathways. It is not unusual for a person to experience a sudden onset of depression when a new carpet is installed or a building is renovated or freshly painted.
Let me explain some basic biochemistry...
In order to detoxify chemical toxins, your body requires adequate amounts of zinc. Zinc runs the enzyme alcohol dehydrogenase and it is this important enzyme that is responsible for detoxifying everyday home and office chemicals. The most common chemical found in carpets, home furnishings, copy machines, secretarial white-out, commercial floor cleaners, polishers, waxes, glues, adhesives, and other common household and office surroundings is a chemical called trichloroethylene.
You may be asking how trichloroethylene can cause depression. Let me explain. When you are exposed to this chemical, it is likely that you either inhaled it or absorbed it through your skin. Normally this chemical, like most chemicals, will be neutralized by your body's detoxification system and eliminated.
However, if body's ability to neutralize chemicals is impaired (possibly a zinc deficiency), the chemical will back up and will accumulate in the brain. When trichloroethylene is stored in the brain it is likely converted to choloral hydrate. If you are a baby-boomer reading this, you may remember the old "Mickey Finn" or knockout drops. And this is exactly how a person feels who is sensitive to tricholoroethylene. They will feel spacey, dizzy, dopey, unable to concentrate, foggy, and very depressed.
I have simply presented one chemical linked to depression. There are other environmental toxins linked to depression. My goal was to provide another piece of the depression mystery.
There is no one treatment that will fix all people. Take ten people suffering with depression and it is likely the cause and the treatment can be different for all ten. What may help one person may do absolutely no good for five others. With that in mind, it is wise to be certain what may be causing your health problem. You may indeed be suffering with a zinc deficiency that would interfere with the body's ability to effectively eliminate chemicals off-gassing from your new carpet.
Again, what works for one will undoubtedly fail on another. With that in mind, it is imperative to have a physician who understands the potential causes of a disease and, for the sake of this report, depression.
Your physician MUST conduct a thorough and rather exhaustive interview/consultation with each patient and determine what direction to go in. For one patient, your physician may determine that an evaluation of the thyroid and cortisol levels would be a good start. For another patient, maybe checking for chemical toxicities and nutrient deficiencies would be the way to go. No matter what, the recommending of an antidepressant without this type of medical detective work is simply not acceptable.
If you think that the cause of your depression is linked to chemical toxicity and/or nutrient deficiencies, then I recommend that you ask your doctor to order the following tests:
RBC mineral/toxic chemical assay (Genova/MetaMetrix)
Toxic Effects Core (Genova/MetaMetrix)
Urine Toxic Metals- DMSA Challenge (Doctor’s Data)
Urine Toxic Metals- DMSA Challenge (Doctor’s Data)
Depression is disease that claims new victims everyday. The causes of this mental disease can range from thyroid, cortisol deficiencies, to nutrient deficiencies/chemical toxicity exposure.
Compliments from Functional Medicine University
www.FunctionalMedicineUniversity.com
References:
1. Rack SK, Makela EH. Hypothyroidism and depression: a therapeutic challenge. Ann Pharmacother. 2000 Oct;34(10):1142-5. 2.Cooke RG, Joffe RT, Levitt AJ. T3 augmentation of antidepressant treatment in T4-replaced thyroid patients. J Clin Psychiatry. 1992 Jan;53(1):16-8. 3.Weissel M. Administration of thyroid hormones in therapy of psychiatric illnesses] Acta Med Austriaca. 1999;26(4):129-31. 4. Hickie I, Bennett B, Mitchell P, Wilhelm K, Orlay W. Clinical and sub- clinical hypothyroidism in patients with chronic and treatment-resistant depression. Aust N Z J Psychiatry. 1996 Apr;30(2):246-52. 5. Haggerty JJ Jr, Prange AJ Jr. Borderline hypothyroidism and depres- sion. Annu Rev Med. 1995;46:37-46. 6. Joffe RT, Levitt AJ. Major depression and subclinical (grade 2) hypo- thyroidism. Psychoneuroendocrinology. 1992 May-Jul;17(2-3):215-21. 7. Pop VJ, Maartens LH, Leusink G, van Son MJ, Knottnerus AA, Ward AM, Metcalfe R, Weetman AP.Are autoimmune thyroid dysfunction and depression related? J Clin Endocrinol Metab. 1998 Sep;83(9):3194-7. 8. Konig F, von Hippel C, Petersdorff T, Kaschka W. Thyroid autoantibod- ies in depressive disorders Acta Med Austriaca. 1999;26(4):126-8. 9. von Zerssen D, Doerr P, Emrich HM, Lund R, Pirke KM. Diurnal variation of mood and the cortisol rhythm in depression and normal states of mind. Eur Arch Psychiatry Neurol Sci. 1987;237(1):36-45. 10. Guechot J, Lepine JP, Cohen C, Fiet J, Lemperiere T, Dreux C. Simple laboratory test of neuroendocrine disturbance in depression: 11 p.m. saliva cortisol. Neuropsychobiology. 1987;18(1):1-4.>/li> 11. Guechot J, Fiet J, Passa P, Villette JM, Gourmel B, Tabuteau F, Cathe- lineau G, Dreux C. Physiological and pathological variations in saliva cortisol. Horm Res. 1982;16(6):357-64. 12. Galard R, Gallart JM, Catalan R, Schwartz S, Arguello JM, Castellanos JM. Salivary cortisol levels and their correlation with plasma ACTH levels in depressed patients before and after the DST. Am J Psychiatry. 1991 Apr;148(4):505-8. 13. Goodyer I, Herbert J, Moor S, Altham P. Cortisol hypersecretion in depressed school-aged children and adolescents. Psychiatry Res. 1991 Jun;37(3):237-44. Foreman DM, Goodyer IM. Salivary cortisol hypersecretion in juvenile depression. J Child Psychol Psychiatry. 1988 May;29(3):311-20. 14.Oldehinkel AJ, van den Berg MD, Flentge F, Bouhuys AL, ter Horst GJ, Ormel J. Urinary free cortisol excretion in elderly persons with minor and major depression. Psychiatry Res. 2001 Oct 10;104(1):39-47. 15. Young AH, Gallagher P, Porter RJ. Elevation of the cortisol-dehydroepiandrosterone ratio in drug-free depressed patients. Am J Psychiatry. 2002 Jul;159(7):1237-9. 16. Twardowska K, Rybakowski J. Limbic-hypo- thalamic-pituitary-adrenal axis in depression: literature review] Psychiatr Pol. 1996 Sep- Oct;30(5):741-55. 17. Maes M, Vandoolaeghe E, Neels H, Demedts P, Wauters A, Meltzer HY, Altamura C, Desnyder R. Lower serum zinc in major depression is a sensitive marker of treatment resistance and of the immune/inflammatory response in that illness. Biol Psychiatry. 1997 Sep 1;42(5):349-58. 18. Rasmussen HH, Mortensen PB, Jensen IW. Depression and magnesium deficiency. Int J Psychiatry Med. 1989;19(1):57-63. 19. Naylor GJ, Smith AH, Bryce-Smith D, Ward NI. Tissue vanadium levels in manic-depressive psychosis. Psychol Med. 1984 Nov;14(4):767- 72. 20. McLoughlin IJ, Hodge JS. Zinc in depres- sive disorder. Acta Psychiatr Scand. 1990 Dec;82(6):451-3. 21. Pfeiffer CC, Braverman ER. Zinc, the brain and behavior. Biol Psychiatry. 1982 Apr;17(4):513- 32. 22. Brodkin CA, Daniell W, Echeverria D, Redlich C, Checkoway H. Concerns and assumptions of labor and management in the dry-cleaning industry. Am J Ind Med. 1999 Oct;36(4):482-3. 23. Echeverria D, White RW, Sampaio C, A behav- ioral evaluation of PCE exposure in patients and dry cleaners: a possible relationship between clinical and preclinical effects, JOEM, 37:6, 667-680, June 1995 24. Moser VC, Cheek BM, MacPhail RC. A multidisciplinary approach to toxicological screening: III. Neurobehavioral toxicity.J Toxi- col Environ Health. 1995 Jun;45(2):173-210. 25. Lemmen CA, Holden CE, Benedek EP. Crimi- nal responsibility and solvent exposure. New Dir Ment Health Serv. 1996 Spring;(69):59-66. 26. Waters EM, Gerstner HB, Huff JE. Trichlo- roethylene. I. An overview. J Toxicol Environ Health. 1977 Jan;2(3):671-707. Review. 27. Winneke G. Acute behavioral effects of expo- sure to some organic solvents -psychophysi- ological aspects. Acta Neurol Scand Suppl. 1982;92:117-29. 28. Kishi R, Harabuchi I, Ikeda T, Katakura Y, Miyake H. Acute effects of trichloroethylene on blood concentrations and performance decre- ments in rats and their relevance to humans. Br J Ind Med. 1993 May;50(5):470-80.
By Gene Bruno, MS, MHS
Are you depressed? If so, you’re not the only one. In fact, approximately 20.9...
